Practice

Mpox: what you need to know
In Practice
We know you want to continue to build on your practice, why not hear from others in the sector striving to do the same.Bookmark
Record learning outcomes
The World Health Organization (WHO) declared mpox a public health emergency of international concern in August, following the spread of a serious strain of the virus, which emerged in the Democratic Republic of the Congo last year.
What is mpox?
Mpox is a viral infection that spreads between people through close contact, and occasionally via objects and surfaces that have been touched by a person with the disease. In settings where the virus is present among animals, it can be transmitted from infected animals to people who have contact with or eat them.
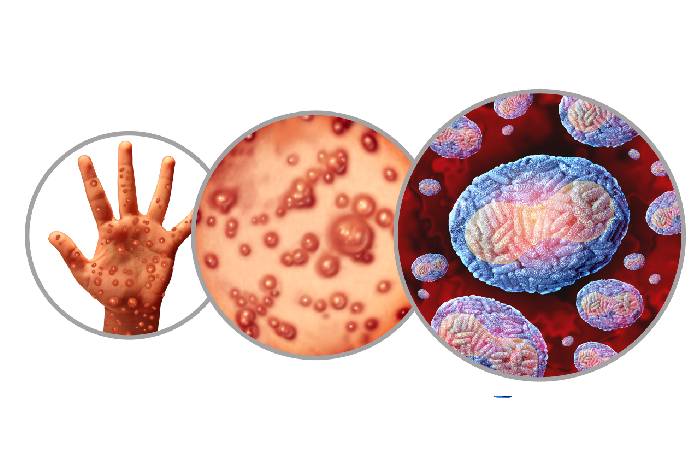
The mpox virus belongs to the Orthopoxvirus genus of the Poxviridae family, which includes variola, the virus that causes smallpox.
Initially known as monkeypox, the preferred term is now ‘mpox’.
What are the symptoms?
Common symptoms include a rash, which may start or be followed by fever, headache, muscle aches, back pain, low energy and swollen lymph nodes. The rash looks like blisters or sores and often starts on the face before spreading to other parts of the body, including the palms of the hands and soles of the feet, the mouth, throat and eyes. It can also start where contact was initially made with an infected person, such as in the anogenital area.
According to WHO, patients can have any number of sores – from one or a few to hundreds or more. Some people may have painful swelling of the rectum, or pain and difficulty when passing urine or when swallowing.
In most cases, symptoms resolve on their own within two to four weeks with self-care such as medication for pain or fever. However, in some people, the illness can be severe or lead to complications such as encephalitis, myocarditis or pneumonia, eye problems, and even death.
Newborn babies, children, people who are pregnant and people with underlying immune deficiencies such as from advanced HIV disease may be at higher risk of more serious mpox disease and death. According to WHO data at the time of writing, between 0.1 and 10 per cent of people with mpox have died.
Who is likely to be at risk?
Anyone who has close contact with someone with mpox is at risk of infection. This includes being face-to-face with an infected person (e.g. talking or breathing close to one another). People who have contact with clothing, bedding, towels, objects and other surfaces that have been touched by someone with mpox are also at risk.
How is the latest outbreak different?
There are two distinct genetic groups (clades) of the mpox virus: clade I (with subclades Ia and Ib) and clade II (with subclades IIa and IIb).
A global outbreak of clade IIb began in 2022 and continues today, including in some African countries where it was initially detected. In August this year, outbreaks of clades Ia and Ib began to affect the Democratic Republic of the Congo and other African countries. Clade Ib has also been detected beyond Africa. Current understanding is that clade I leads to more severe disease and death than clade II, says WHO.
Health officials have now reported the UK’s first instance of clade Ib mpox although there have been many cases of clade II disease in this country.
What should I do if I suspect a case?
Mpox is a notifiable disease, so you should contact your local health protection team by phone and advise the patient to consult their GP. Diagnostic testing is available in UK Health Security Agency (UKHSA) laboratories, some NHS laboratories, and certain private labs too.
In September, the NHS issued ‘action cards’ for healthcare professionals to use in the event of a person presenting with possible symptoms. Community Pharmacy England says the primary care providers’ action card is something “pharmacy owners will want to read, ensuring their teams are aware of the key points”.
Reducing the risk
Anyone with suspected mpox should isolate from others until they have been evaluated and tested. Infected patients should isolate from others until all lesions have crusted over, the scabs have fallen off and a new layer of skin has formed. Condoms should be used as a precaution during sex for 12 weeks after recovery.
What is the treatment for mpox?
Anyone with mpox who is recovering at home should stay hydrated, eat well and get sufficient sleep. Patients should avoid scratching their skin and should take care of their rash by cleaning their hands before and after touching lesions and keeping skin dry and uncovered – unless they are in a room with someone else, in which case they should cover it with clothing or a bandage.
The rash can be kept clean with sterilised water or antiseptic. Saline rinses can ease sores in the mouth, and warm baths with baking soda and Epsom salts can relieve the discomfort of sores on the body. Paracetamol can help manage pain caused by lesions, if needed.
People with severe mpox may require hospitalisation and treatment with antiviral medicines. An antiviral developed to treat smallpox (tecovirimat) was approved in January 2022 by the European Medicines Agency for the treatment of mpox in exceptional circumstances.
Is there an mpox vaccine?
As the mpox virus is similar to the smallpox virus, smallpox vaccines can offer a degree of protection against it. The UKHSA and the Joint Committee on Vaccination and Immunisation recommends the use of the MVA (Modified Vaccinia Ankara) vaccine.
Currently, the NHS is offering vaccines to people who are most likely to be exposed to mpox via a vaccination programme in London and Greater Manchester.
Advice for travellers
The UKHSA says the risk to most travellers is low and vaccination against mpox is not recommended for most people. However, it does advise that anyone who is planning to travel to an affected country checks the Government’s latest travel advice online.
Useful resources
- A list of countries affected by mpox clade I is available from the UK Health Security Agency
- The Department of Health’s Travel Health Pro website has current information about mpox and its prevalence
- The NHS offers information about mpox